最新 soap notes meaning Soap notes meaning Whether covered by insurance or not, good clinical notes support the rationale for treatment and are necessary should there be a lawsuit or medical issue that requires the patient record be examined The following is an explanation in lay terms as toSOAP Method 30 Minute Devotionals With Meaning SOAP Steps 1The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission noteSOAP acronym for subjective data, objective data, assessment, plan, the way the progress notes are organized in problemoriented recordkeeping soap sōp any compound of one or more fatty acids, or their equivalents, with an alkali Soap is detergent and used as a cleanser

Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki
S.o.a.p notes meaning
S.o.a.p notes meaning-O– The O stands for observation what do you see in the verses that you're reading?√ダウンロード soap notes meaning What does soap notes mean A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that The term chiropractic "SOAP notes" has nothing to do with working up a lather So what does "SOAP" stand for?SOAP (an acronym for Subjective,



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
Find out what is the full meaning of POS on Abbreviationscom!What is a SOAP Note – Definition A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that are used by professionals in the health sector The SOAP note is usually included in the patient's medical record for the purpose of informing any otherWhen confronted with a reading passage or document, students need a process to help them begin to determine the purpose or significance of the document It will then be much easier to interpret or even gather evidence from the document when students have a literacy tool to help them begin the process
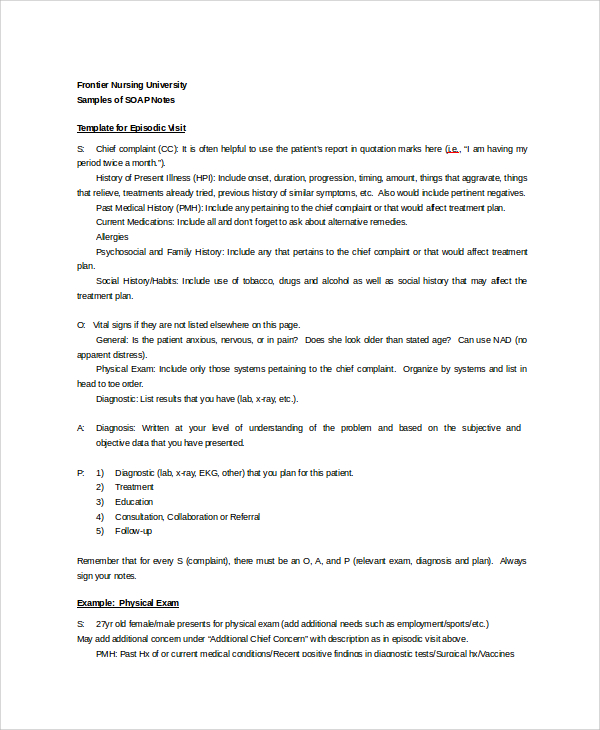
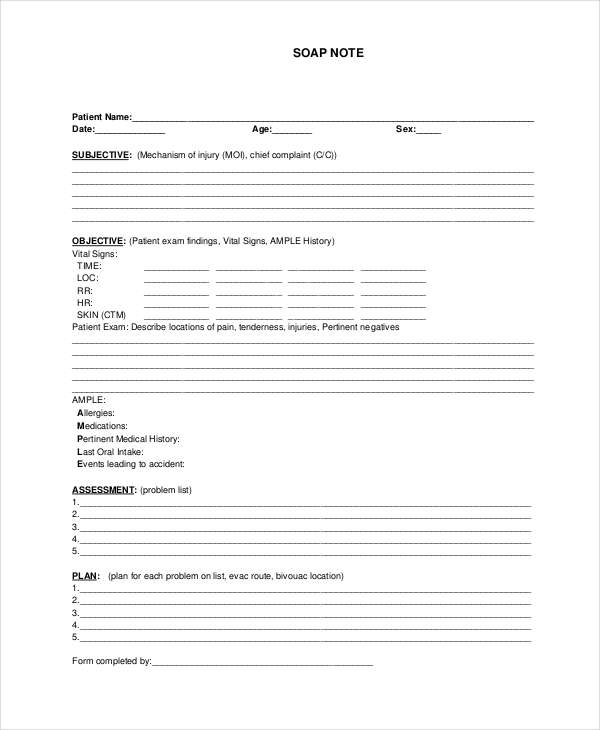
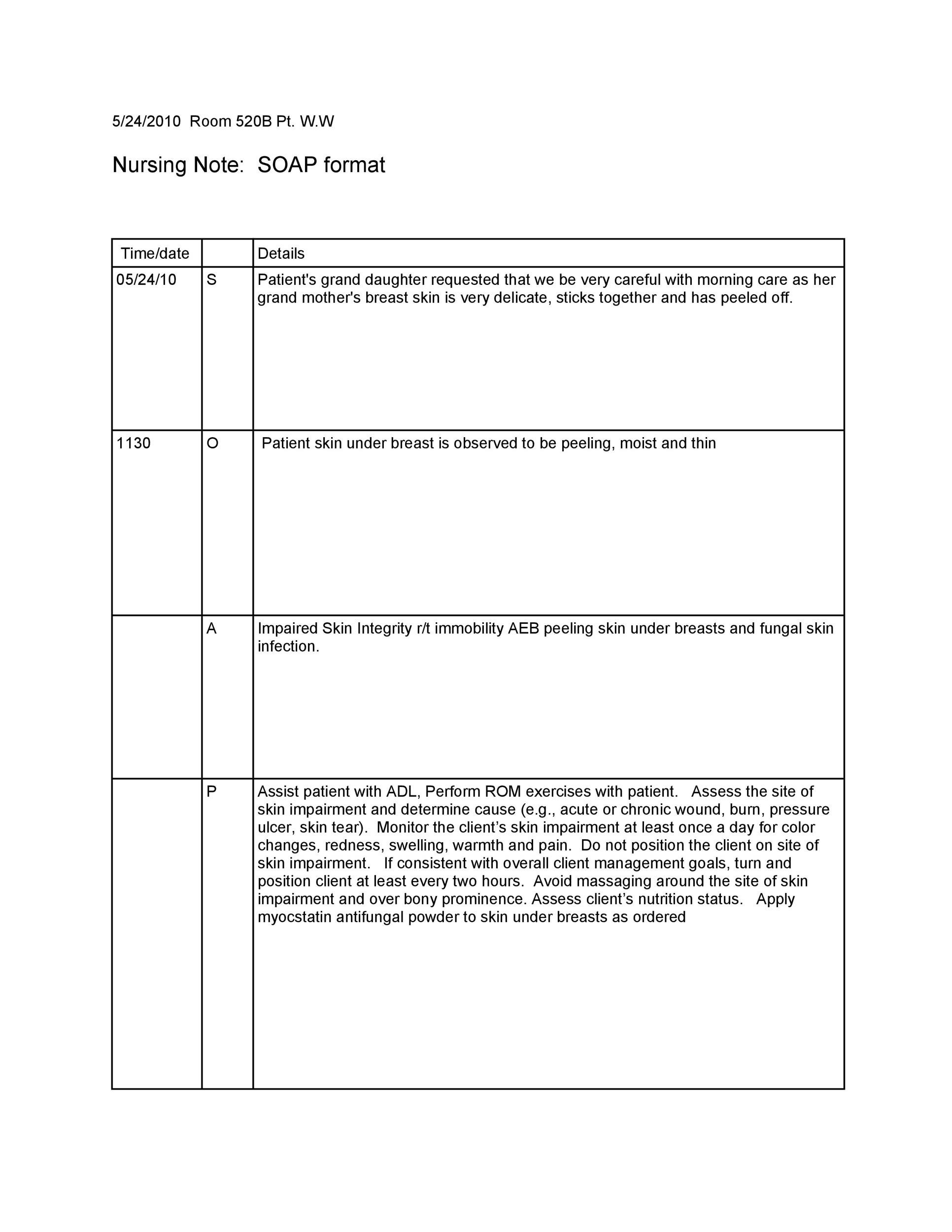
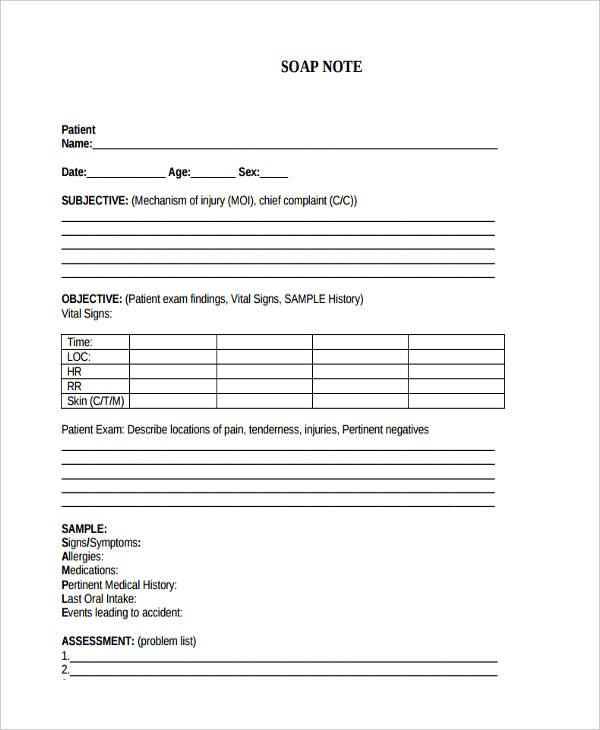
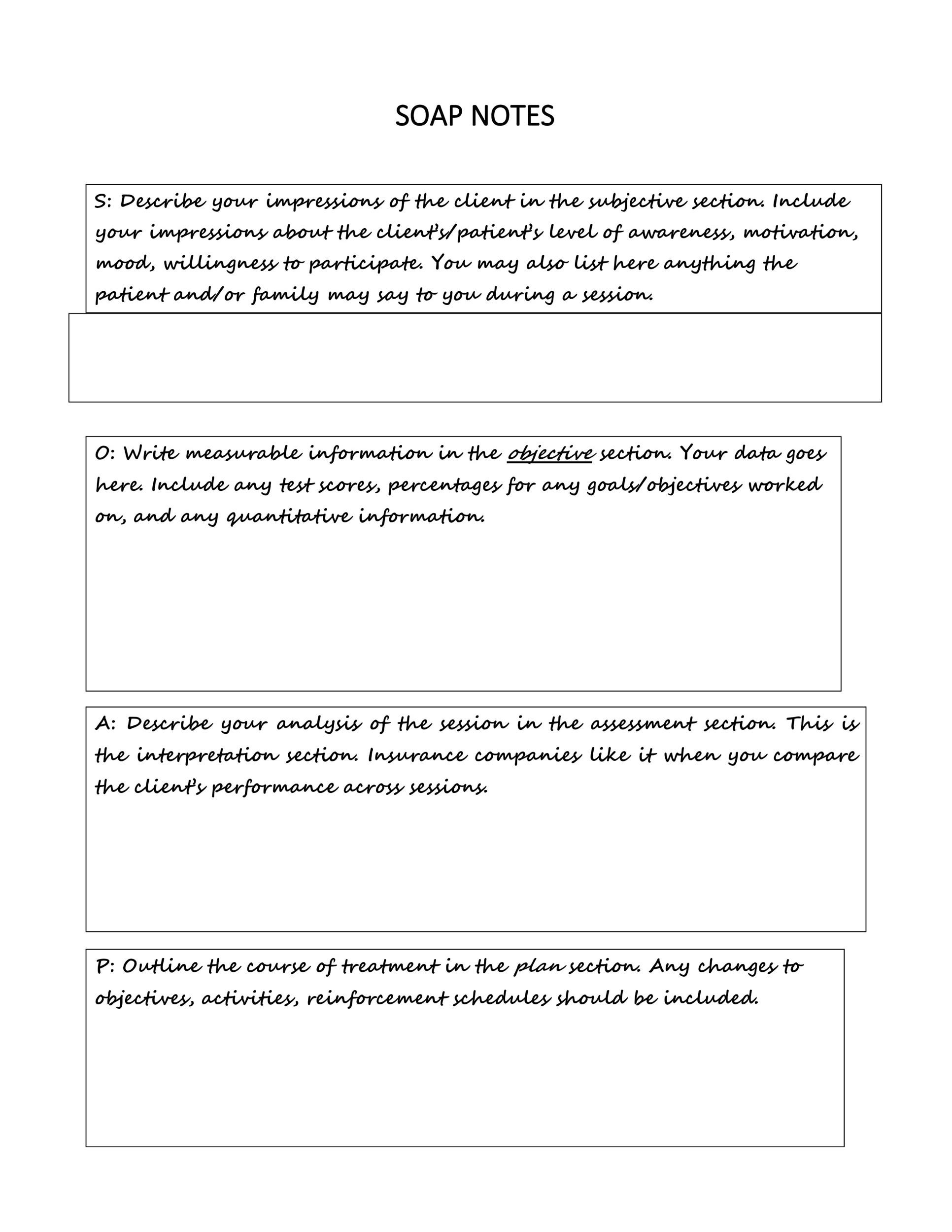
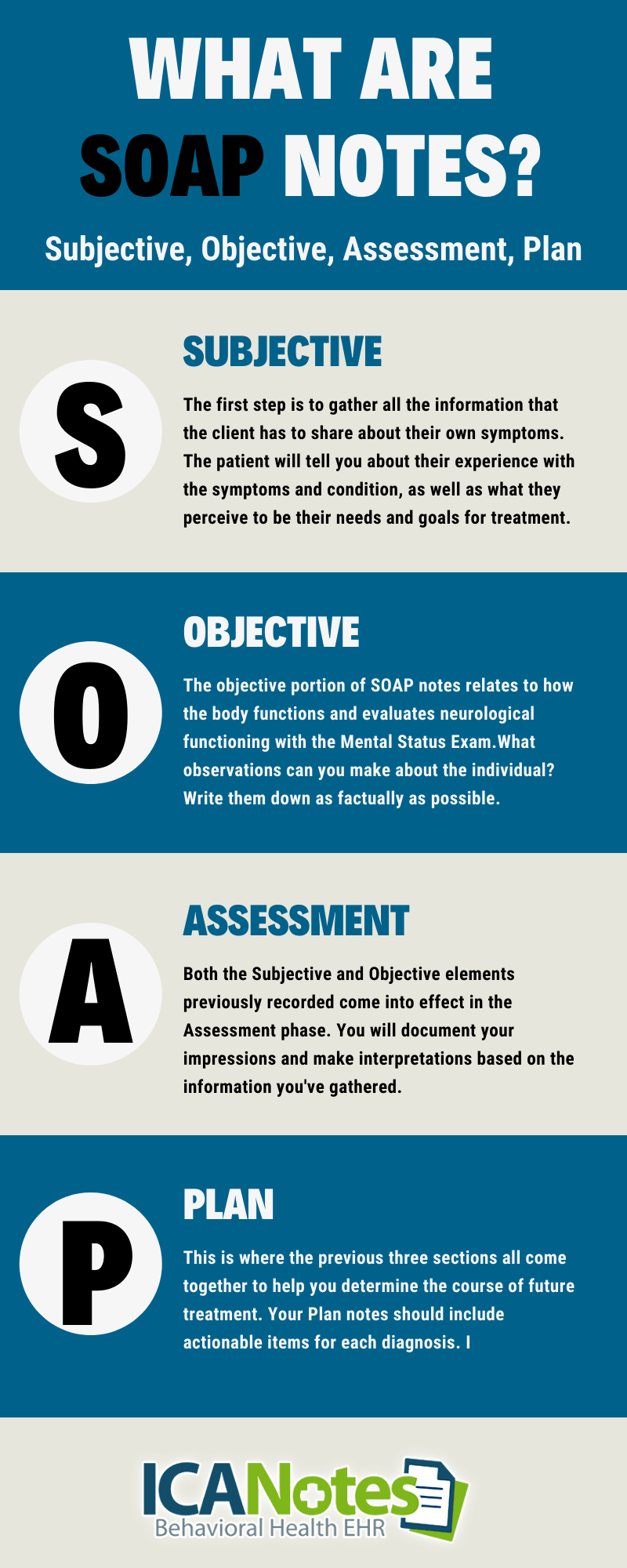
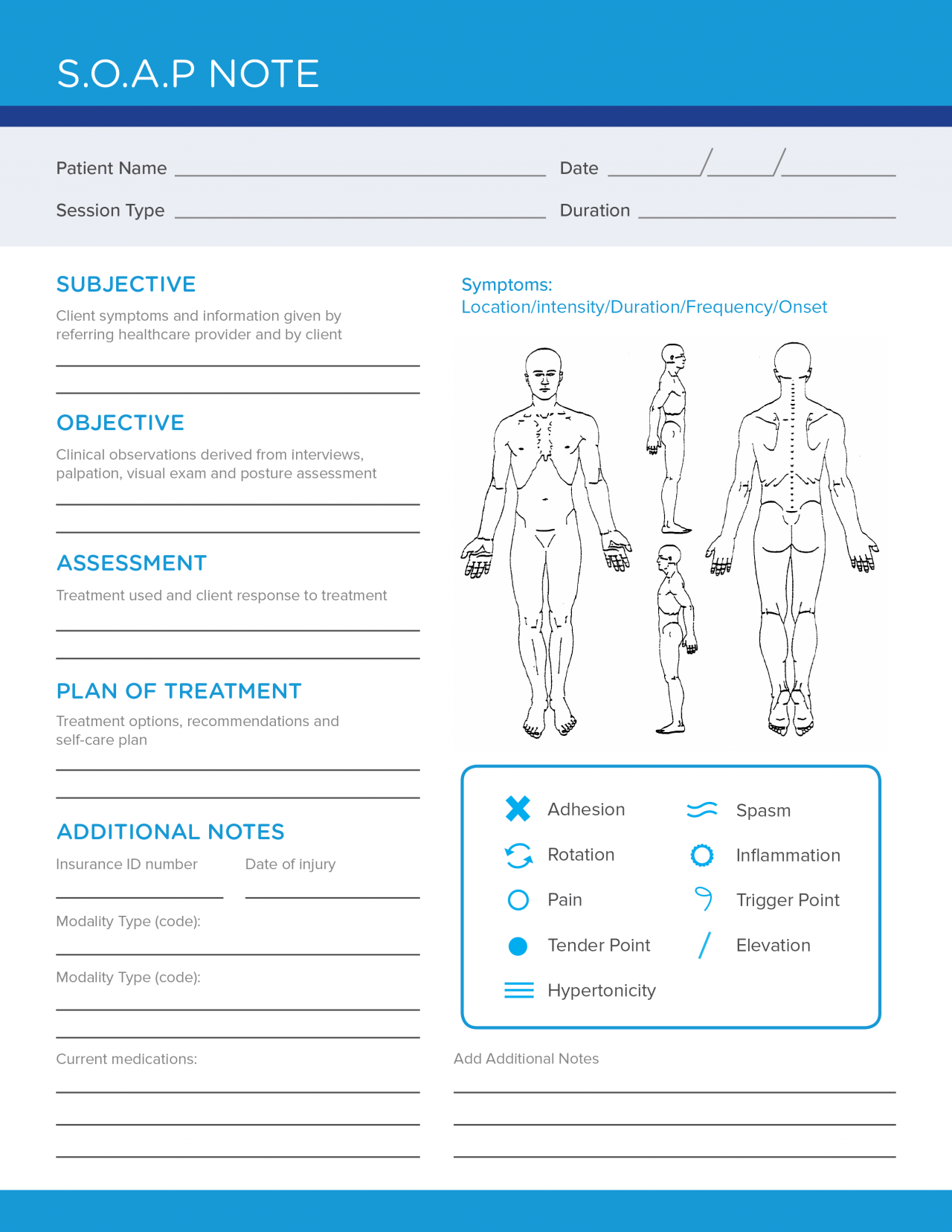
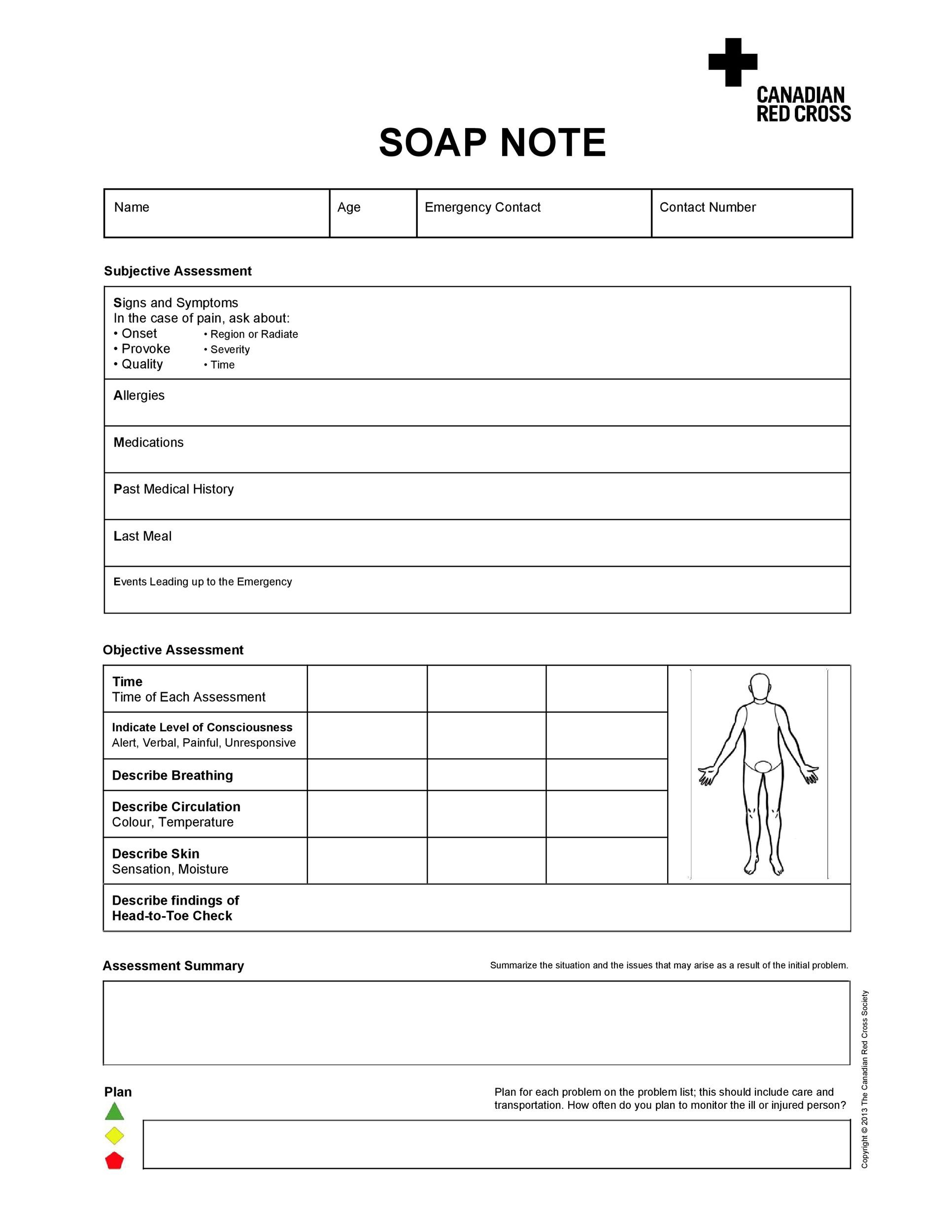
A SOAP note is basically a method of documentation that medical professionals employ to record a patient's progress during treatment Health care providers can use it to communicate the status of a patient to other practitioners, giving them a cognitive framework that they can refer to, upon assessment There are four components of the note, namely Subjective Upon medicalSOAP Student Organization for Activity Planning (Salisbury State University) SOAP Summary On A Page SOAP Systems/Operations Analysis of Programs SOAP Systems for Oceanic Analysis and Prediction SOAP Supertanker Operational Assessment Project SOAP SIM Over the Air Programming (wireless telecommunications) SOAP Spine, Orthopedic andSOAP notes gave physicians structure and a way for practices to communicate with each other, a notion that is still transforming the industry It was the initial users of SOAP notes who were able to retrieve patient records for a given medical problem the fastest – something EHRs do even better today Similar to how EHR software has improved the way providers find patient charts
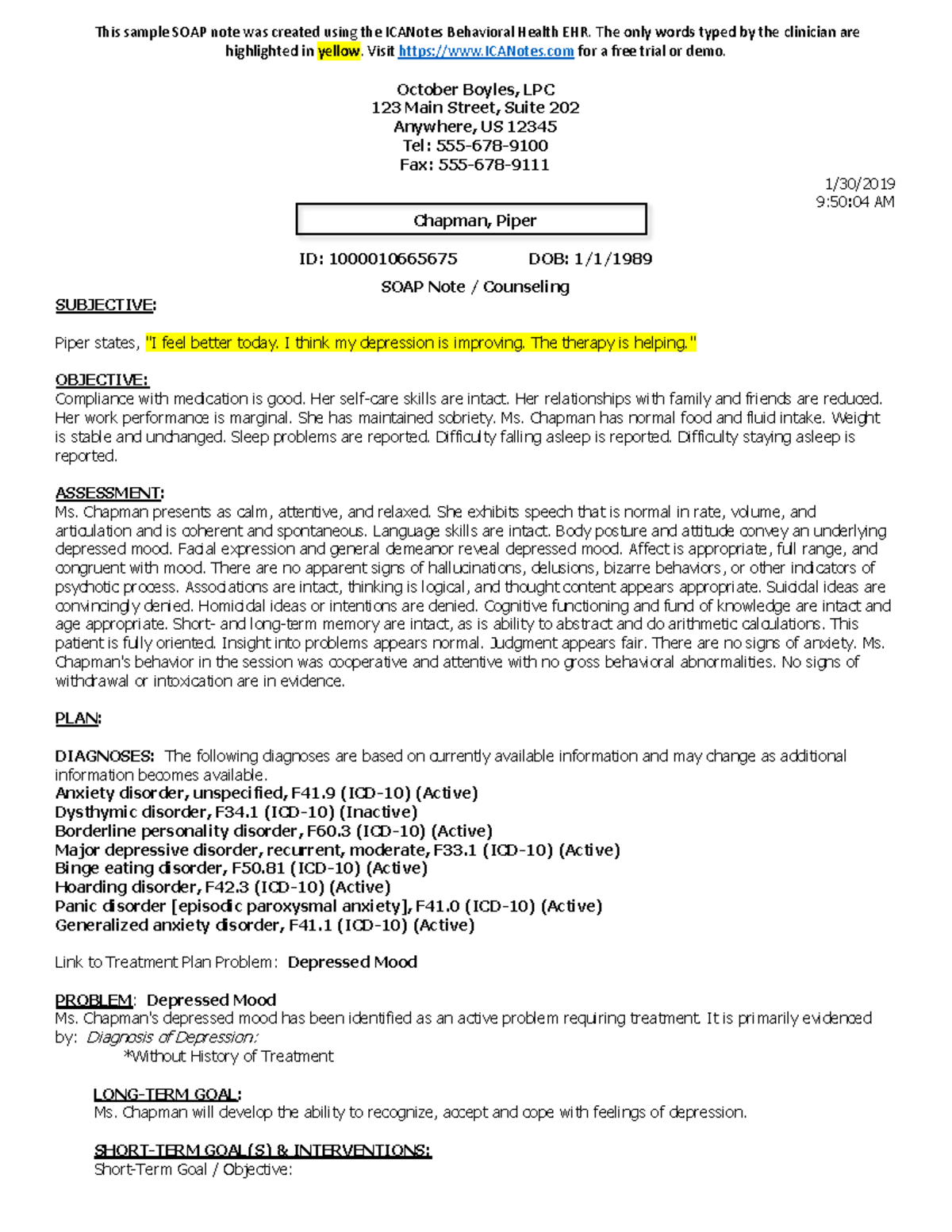
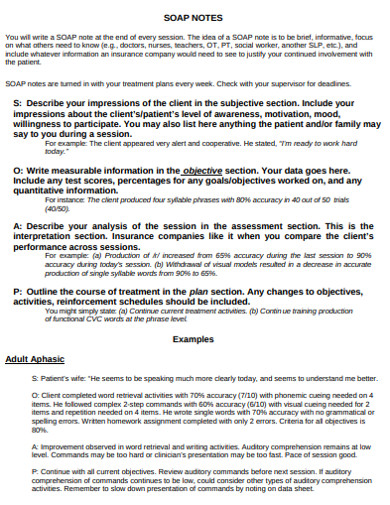
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers The SOAP note is a way for healthcare workers to document in a structured and organized way123 SOAP (Subjective, Objective, Assessment, Plan) notes are an essential component of providing care and treatment for patients I t ' s vital to document data and information from every patient encounter T herapists must use SOAP notes to monitor and document patient progress, log services, and communicate patient information to other professionalsCe service gratuit de Google traduit instantanément des mots, des expressions et des pages Web du français vers plus de 100 autres langues




Writing Soap Notes Step By Step Examples Templates



Free 15 Soap Note Templates In Pdf Ms Word
3 Journal using SOAP method (10 minutes) a S = Scripture Write down a meaningful scripture from your reading b O = Observation write 12 paragraph "Observation" about this passage c A = Application Write a 12 paragraph of personal "Application" about this passage d P = Prayer 4 Share or pray over you thoughts (5 minutes) Notes 1 Make sure you use at least one page in If you are required to write your case notes in SOAP note format this post will give you an example of some of the most important components to include your SOAP note formated case note S Subjective Data Includes – Clinically important statements made by client or family members attending session Statements may refer to feelings, thoughtsList of 1 best SOAP NOTES meaning form based on popularity Most common SOAP NOTES abbreviation full form updated in June 21




Medical Terminology And Abbrev Pages 1 10 Flip Pdf Download Fliphtml5



How To Document A Patient Assessment Soap Geeky Medics
SOAP documentation SOAP documentation is a problemoriented technique whereby the nurse identifies and lists the patient's health concerns It is commonly used in primary healthcare settings Documentation is generally organized according to the following headings S = subjective data Example What is the patient experiencing or feeling, how long has this been an issue, what SOAP is an acronym Subjective, Objective, Assessment, and Plan This system was created to help prevent charting mistakes or information from being left out Just like each patient is unique, each chart in unique with information and length of notes Here is an example what each letter of SOAP includes S SubjectiveS– The S stands for Scripture you physically write out the scriptureyou'll be amazed that what God will reveal to you just by taking the time to slow down and actually write out what you are reading!



Soap Note And Documentation Templates Examples Seniors Flourish



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software
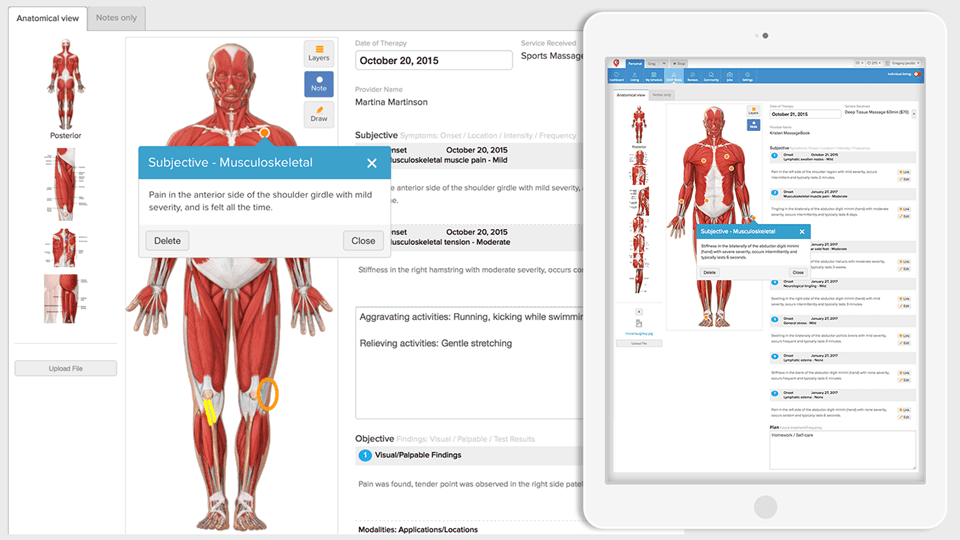
Since all SOAP notes follow the same structure, all your information is clearly laid out in digestible parts, making it easy for any provider—including yourself—to read the note at a later date and know exactly what's going on in a client's treatment plan These notes should be brief, focused, informative, and always in the past tense As you write more notes, you'll find a system DAP vs SOAP Notes If you have ever taken progress notes as an employee of a large organization, you may have been asked to use the SOAP format The SOAP (Subjective, Objective, Assessment and Plan) note is probably the most popular format of progress note and is used in almost all medical settings The main difference between the SOAP and DAP notes is that the A SOAP note is a documentation format that massage therapists and other healthcare workers use to document client encounters SOAP is an acronym that stands for subjective, objective, assessment and plan



3



How To Write A Soap Note
A SOAP ( s ubjective, o bjective, a ssessment, p lan) note is a method of documentation used specifically by healthcare providers SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way SOAP notes are a popular format for healthcare documentation and are used across the spectrum of healthcare services 1 Document in the note a patient statement or what the patient observes The "S" in SOAP stands for subjective, so this part of the documentation is related to the patient's observations of her own symptoms or a complaint about some ailment It is SOAP NOTE 101 Most mental health clinicians utilize a format known as SOAP notes SOAP is an acronym that stands for S – Subjective O – Objective A – Assessment P – Plan A SOAP note is a progress note that contains specific information in a specific format that allows the reader to gather information about each aspect of the session Start 30Day TheraPlatform Free Trial to




How To Write A Soap Note With Obstetric Examples Healthproadvice




Free Soap Note Templates How To Write Examples Safetyculture
Progress note Progress notes are written in a variety of formats and detail, depending on the clinical situation at hand and the information the clinician wishes to record One example is the SOAP note, where the note is organizedSAP Satisfactory Academic Progress SAP Systems Applications and Products (data processing) SAP Session Announcement Protocol SAP Student Assistance Program SAP Standard Assessment Procedure (energy cost measurement;The SOAP note stands for Subjective, Objective, Assessment, and Plan This note is widely used in medical industry Doctors and nurses use SOAP note to document and record the patient's condition and status The SOAP note is considered as the most effective and standard documentation used in the medical industry along with the progress note




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd



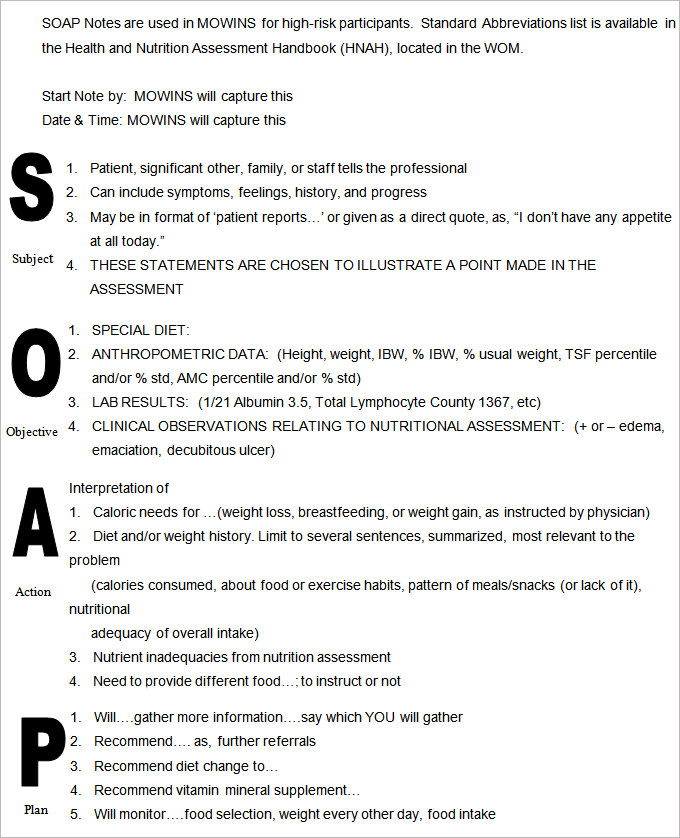
Nutritional Progress Notes Ppt Video Online Download
Who is the audience?'Point Of Sale' is one option get in to view more @ The Web's largest and most authoritative acronyms and abbreviations resourceA SOAP note is information about the patient, which is written or presented in a specific order, which includes certain components SOAP notes are used for admission notes, medical histories and other documents in a patient's chart Many hospitals use electronic medical records, which often have templates that plug information into a




Writing Soap Notes Step By Step Examples Templates




What Are Soap Notes Acucharting
SOAPS Why use SOAPS when interpreting Primary Source documents?Recovery SOAP NOTES abbreviation meaning defined here What does SOAP NOTES stand for in Recovery?What does SOAP NOTES abbreviation stand for?



Free 28 Note Templates Examples In Pdf Doc Examples
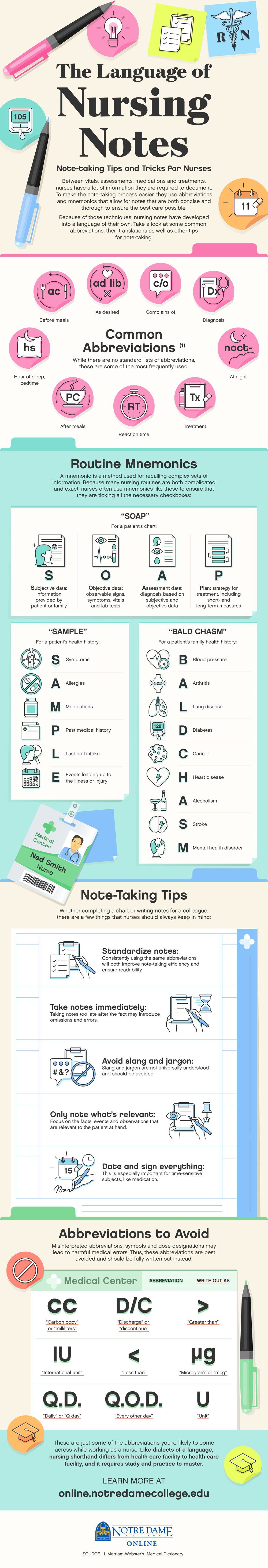



The Language Of Nursing Notes Mnemonics Notre Dame College Online
What is a SOAP Note? A SOAP note, or a subjective, objective, assessment, and plan note, contains information about a patient that can be passed on to other healthcare professionals To write a SOAP note, start with a section that outlines the patient's symptoms and medical history, which will be the subjective portion of the note After that section, record the patient's vital signs andTreatment Notes and Progress Notes Using a Modified SOAP soap notes meaning ,The SOAP note is a commonly used format and is one with which most medical personnel are familiar (see Chapter 2 for the history and development of the SOAP note) The SOAP format is relatively easy to master and provides a quick format for writing a treatment note This chapter presents a format



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Soap Note
The SOAP Acronym SOAP is an acronym for the 4 sections, or headings, that each progress note contains Subjective Where a client's subjective experiences, feelings, or perspectives are recorded This might include subjective information from a patient's guardian or someone else involved in their care Objective For a more complete overview of a client's healthDefinitions of s o a p, synonyms, antonyms, derivatives of s o a p, analogical dictionary of s o a p (English) Lettris is a curious tetrisclone game where all the bricks have the same square shape but different content Each square carries a letter To make squares disappear and save space for other squares you have to assemble English words (left, right, up, down) from the falling squaresGet the top SOAP NOTES abbreviation related to Recovery




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Soap Note Examples Soap Note Occupational Therapy Quotes Occupational Therapy Activities
What does SOAP mean? In a previous post, we reviewed the necessity of basic best practices for SOAP notes including legibility, identification, and dated chart entries In this post, we review the proper structure and contents of a SOAP note The acronym SOAP stands for Subjective, Objective, Assessment, and Plan Each category is described below S = Subjective or symptoms andIs there a repetition of words?




Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




How To Write Massage Therapy Soap Notes Mblexguide
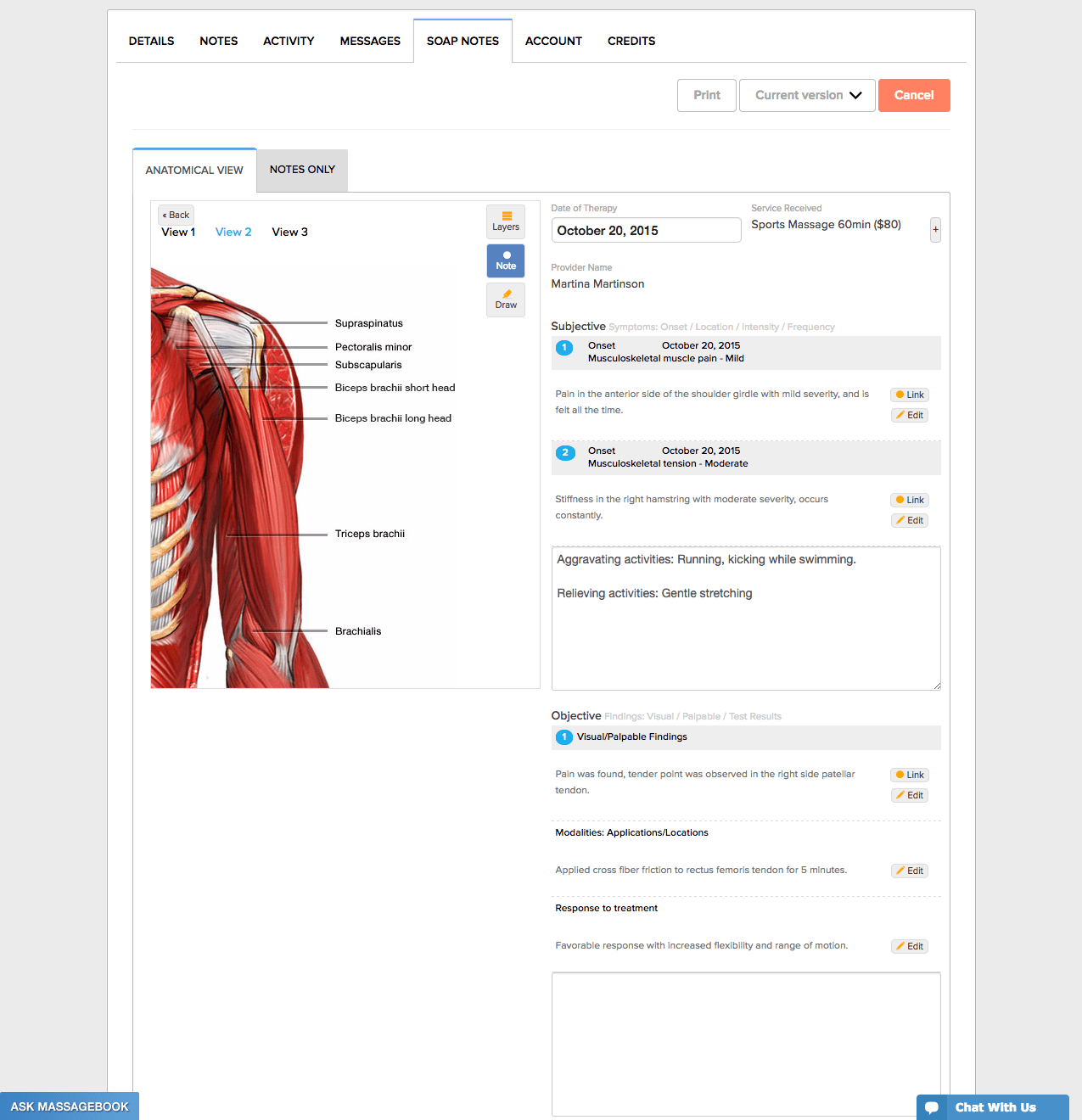
Introduction The SOAP Note Template is a documentation method used by medical practitioners to assess a patient's condition It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information Developed by Dr/ Lawrence Weed in the 1960s, the SOAP Note Template methodology records vital patient medical SOAP Notes Dentistry Example 1 Chief Complaint 23 year old male presents w/ a chief complaint of "my lower left back jaw has been sore for the past few days"S History of Present Illness Pt relates history of swelling for past 3 days, asymptomatic previously Medical History Med Conditions Medications Allergies Past Sx Social Hx Asthma Albuterol None Ear Lac 09 Using SOAP is good medicine Michael H Riegger, DVM, DABVP We all see these articles about what it takes to run a successful practice slick marketing, conflict management, Web pages, team training, appropriate compensation packages, etc The list is endless "You get the best out of others when you give the best of yourself"




Client Intake Forms Agreements Acuity Scheduling




Understanding Soap Format For Clinical Rounds Global Pre Meds
DAILY PROGRESS NOTES SOAP Note Format soap notes meaning ,The term "SOAP notes" refers to a particular format of recording information regarding treatment procedures Documentation of treatment is an extremely important part of the treatment process In virtually *all* e mployment settings, some form of documentation is required and SOAP notes are the SOAP notes are a way for nurses to organize information about patients SOAP stands for subjective, objective, assessment and plan Nurses make notes for each of these elements in order to provideUK) SAP Substance Abuse Professional SAP Soon As Possible SAP SupportaProject SAP Single Assessment Process




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice
.png)



Free Massage Soap Notes Forms Massagebook
印刷可能 soap meaning medical Soap meaning medical Here is a personal example Colossians 158 S– The faith and love that spring from the hope that is stored up for you in heaven and that you have already heard about in the word of truth, the gospel that has come to youAll over the world this gospel is bearing fruit and growing, just as it has been doing among SOAP notes are easy to use and designed to communicate the most relevant information about the individual They can also provide documentation of progress For clinical professionals, SOAP notes offer a clear, concise picture of where the client is at the time of each session They contribute to the continuity of care and are a tool for risk management andS O A P NOTE S = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session 1 If adding your own explanatory information, place within brackets to make it clear that it is not a direct quote



Tips For Writing Better Mental Health Soap Notes Updated 21




Pdf Clinical Note Taking Is Very Challenging For Many Students That Are Novice In The Field Many Times Even Professionals Ask What Type Of Note Taking Is Easy For You So I
The SOAP note (Subjective, Objective, Assessment, and Plan) is a basic template for documentation employed by health care providers to write out notes in a patient's chart It has four sections A closer examination and dissection of the SOAP note format is key to understanding how doctors think A thorough understanding of this tool makes it clear why "BS" could mean "bloodLooking for the definition of POS?SOAP notes are intended to capture specific information about a client and certain aspects of the session SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning) All SOAP notes should




How To Write Incredible Physical Therapist Soap Notes



Soap Note Writing Tips For Mental Health Counselors Youtube



Www Nbome Org Docs Peorientationguide Pdf



Counseling Soap Note Example Warning Tt Undefined Function 32 This Sample Soap Note Was Created Studocu




How To Write A Soap Note With Pictures Wikihow




College Certificate Programs Certificateprograms Occupational Therapy Quotes Soap Note Occupational Therapy Activities




Quiz Worksheet Soap Notes In Nursing Study Com




Writing Soap Notes Step By Step Examples Templates



1



What Are The Four Parts Of A Soap Note Slide Share




Dap Vs Soap For Counselors Therapists




Free Soap Notes Templates For Busy Healthcare Professionals



Free 14 Blank Note Examples In Pdf Examples



1



Pharmacy Oregonstate Edu Sites Pharmacy Oregonstate Edu Files Soap Rubric And Components Final Nov 17 Pdf



Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook



Www Nbome Org Wordpress Wp Content Uploads 17 03 Comlex Usa L2pe Orientation Guide Website 19 Pdf




Soap Notes Youtube




Examples Of Soap Notes In Nursing Video Lesson Transcript Study Com




Aba Practice Daily Simple Guidelines For Writing Soap Notes



Www Sausd Us Cms Lib Ca Centricity Domain 4950 2 71 soap read Pdf



Soap Notes For Massage Therapy




Soap Notes Resources Digital Chalkboard




51 Sample Soap Notes In Pdf Ms Word Excel
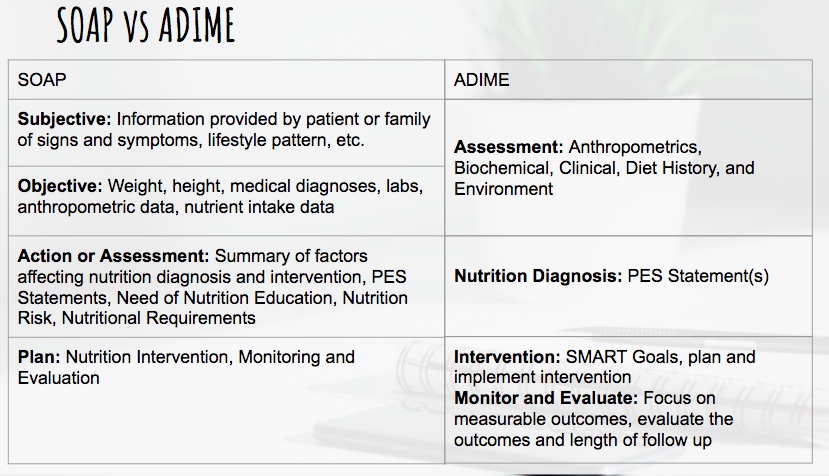



Dietetics Nutritioncare Clinical Documentation 18 Ubc Wiki




Transitioning To Soap 2 0 Webpt Emr Help




How To Write Incredible Physical Therapist Soap Notes




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




Mental Health Marketing Company Behavioral Health Marketing Therapistx




Jm Rom Pdf Anatomical Terms Of Motion Musculoskeletal System



Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook




Documentation Of Pharmaceutical Care Ppt Download
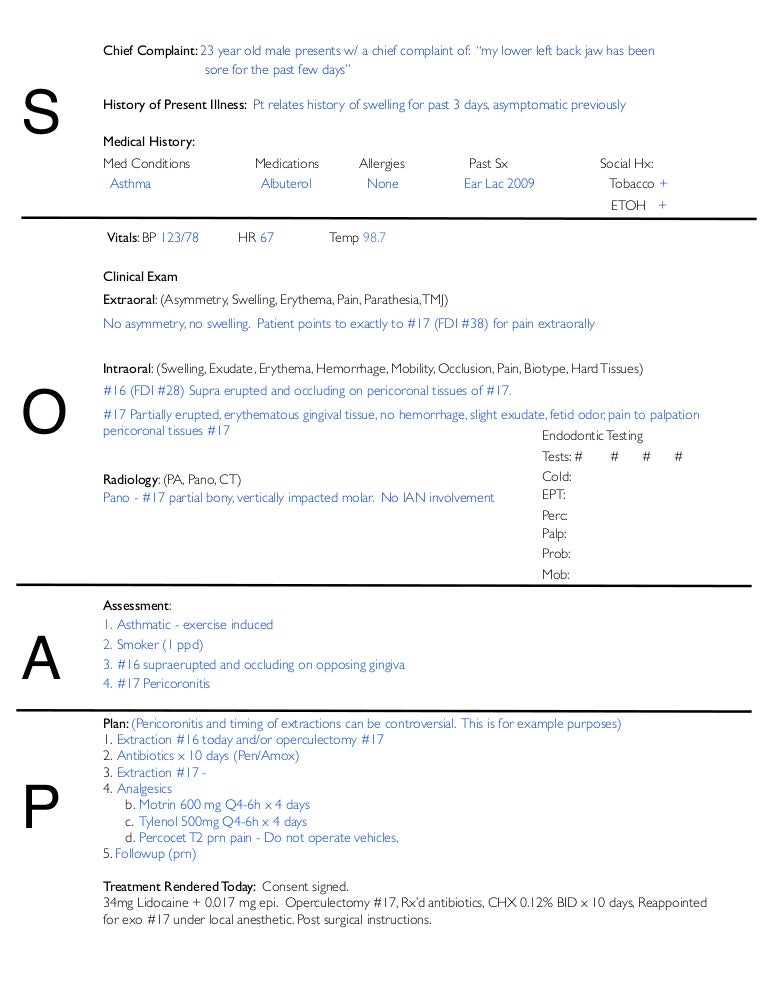



Soap Notes Dentistry Example



How To Take Clinical Notes Using Da R P
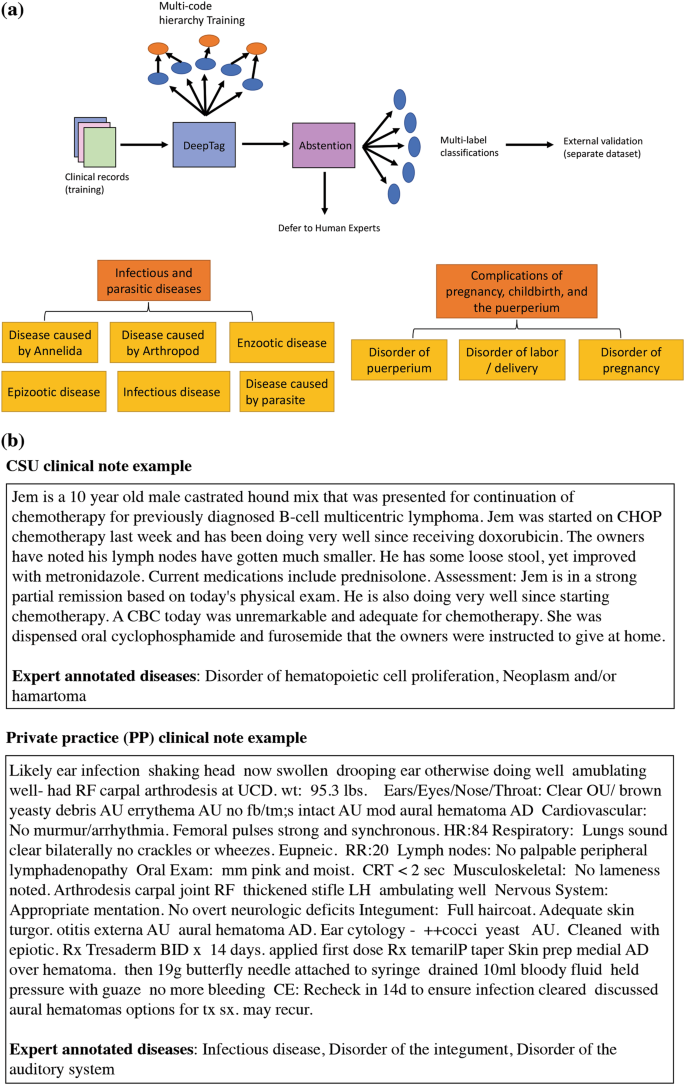



Deeptag Inferring Diagnoses From Veterinary Clinical Notes Npj Digital Medicine




How To Write A Soap Note



Which Fragrances Have The Best Meaning Polarizing And Entertaining Reviews On Fragrantica Fragrance



40 Fantastic Soap Note Examples Templates ᐅ Templatelab



Soap Notes Meaning



The Language Of Nursing Notes Mnemonics Notre Dame College Online




Documentation And Coding Practices For Risk Adjustment And Hierarchical Condition Categories



What Are Soap Notes In Counseling Examples




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd




Rop Sports Medicine Lecture 5 S O A P Notes Ppt Video Online Download




Heart Failure Soap Note Pdf Heart Failure Internal Medicine



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Free Soap Notes Templates For Busy Healthcare Professionals




Write An Amazing Occupational Therapy Soap Note With Example Myotspot Com




Saykara Ai Assistant For Physicians



1




Write An Amazing Occupational Therapy Soap Note With Example Myotspot Com




How To Write Massage Therapy Soap Notes Mblexguide



Physical Therapy Soap Note Example Therapy Daily Note



Types Of Notes Therapists Use And What To Include In Therapy Notes Master Class Ch 3



Snac Soap Notes Across The Curriculum By Acronymsandslang Com
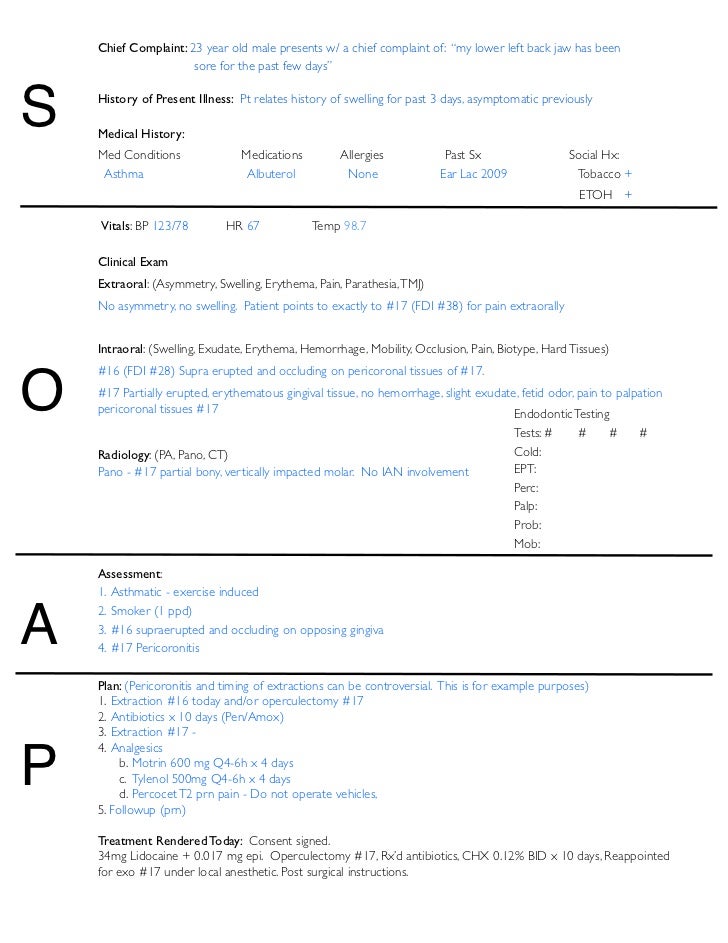



Soap Notes Dentistry Example




Crafting The Ideal Ot Note Ot Potential




Free Easy To Use Massage Therapy Soap Notes Massagebook Massagebook
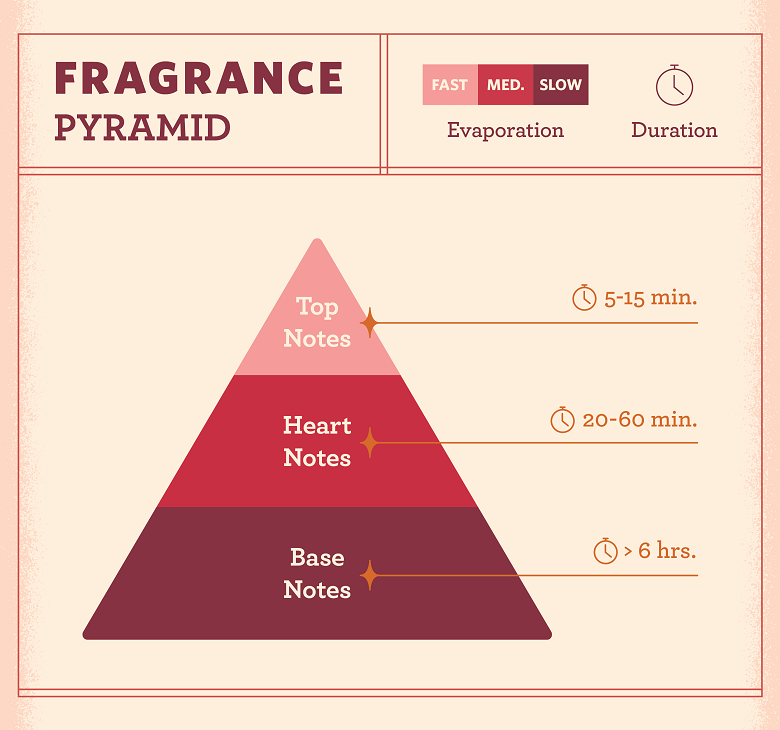



Fragrance Notes Everything You Need To Know Fragrancex
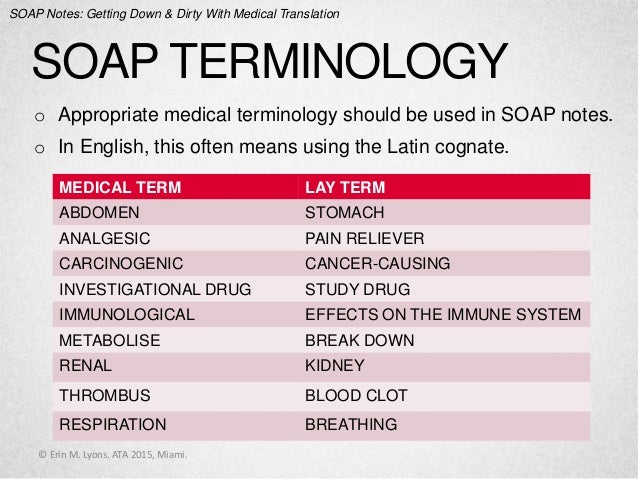



Soap Notes Getting Down And Dirty With Medical Translation




Free Soap Note Templates How To Write Examples Safetyculture




What Is Soap Notes The Benefits Of Standardized Notes Cybernet Blog



Health Science Self Guided Soap Notes Exploration By Laura Miller




What Are Soap Notes In Counseling Examples




What Is A Soap Note Jess Brantner Wvu Dietetic Intern
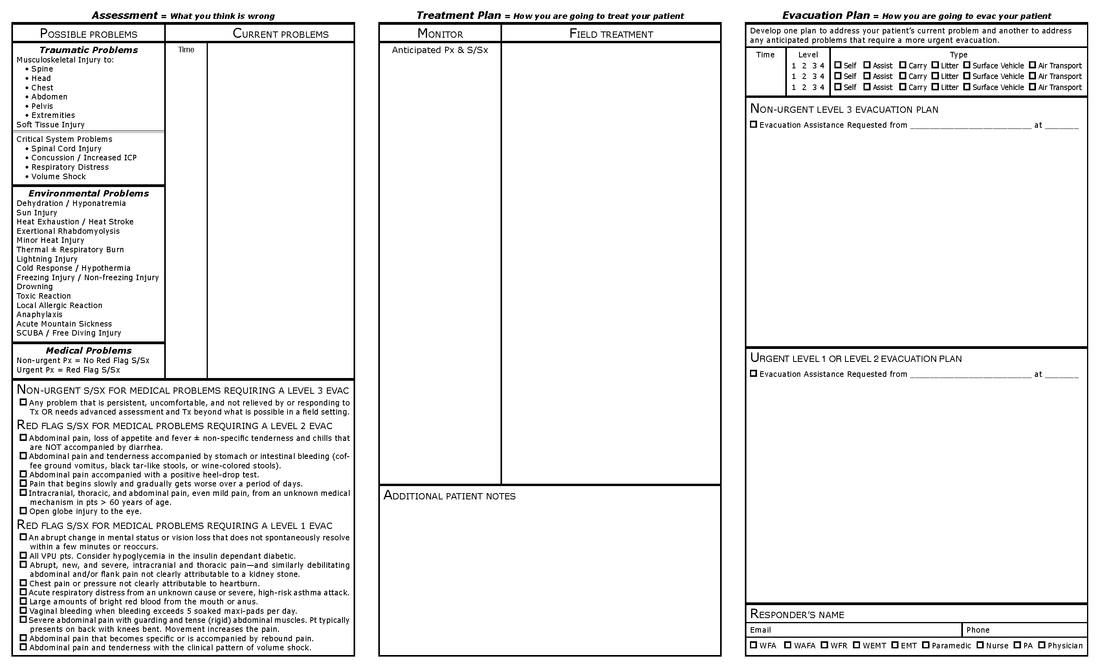



Wilderness Medicine Training Center S Patient Soap Notes




Soap 2 0 Faq Webpt Emr Help



Module Three Documentation Of Slp Services In Different Settings




Soap Notes The St John S Pa Program Survival Guide




How To Write A Soap Note For Mental Health How To Write A Soap Note With Pictures




What Are Psychotherapy Notes Vs Progress Notes Theranest



How To Write A Soap Note Occupational Therapy
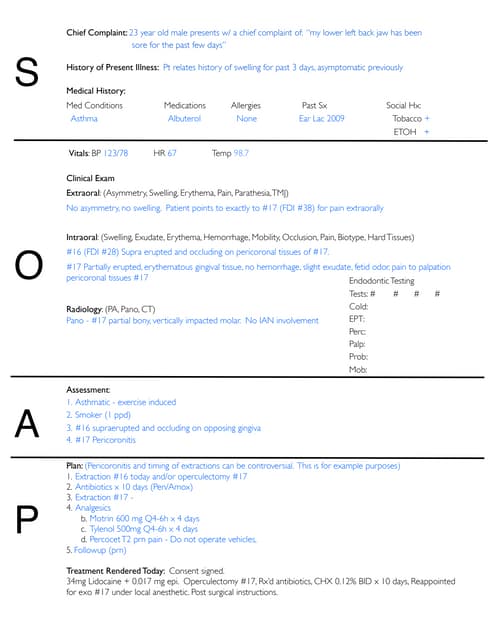



Soap Notes Dentistry Example




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice




Soap Notes




Step By Step Guide On Sap Support Backbone Update And Enabling Note Assistant For Digitally Signed Sap Notes Sap Blogs



0 件のコメント:
コメントを投稿